


Advanced Eye Medical Orange County Lasik and Cataract Surgery
The trusted Orange County eye surgery specialists at Advanced Eye Medical Group have the experience that matters when it comes to helping you achieve the best vision & results possible. Now in our fourth decade of serving the Orange County community, we look forward to counting you among our thousands of satisfied patients with the absolute best laser eye surgery in the area.
Quick Contact Form
OUR SERVICES
About Us

Faris R. Ghosheh, M.D.
Dr. Faris Ghosheh specializes in corneal transplantation, cataracts and refractive surgery. He graduated Cum Laude from UC Irvine earning …
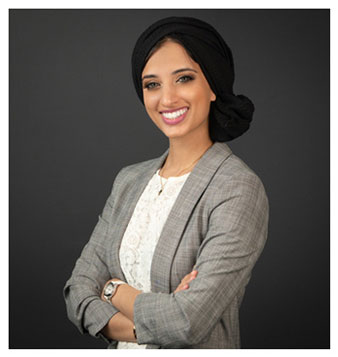
Dr. Sarah Ahmed, M.D.
Sarah Farukhi Ahmed, MD is an ophthalmologist and glaucoma surgeon. She graduated Magna Cum Laude from the University of ..
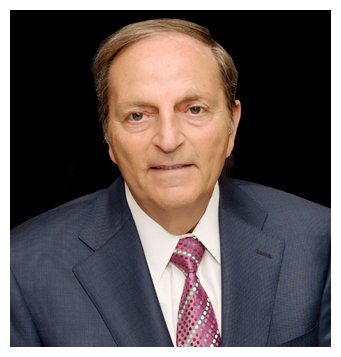
R.K. Ghosheh, M.D.

Faris R. Ghosheh, M.D.
Dr. Faris Ghosheh specializes in corneal transplantation, cataracts and refractive surgery. He graduated Cum Laude from UC Irvine earning …
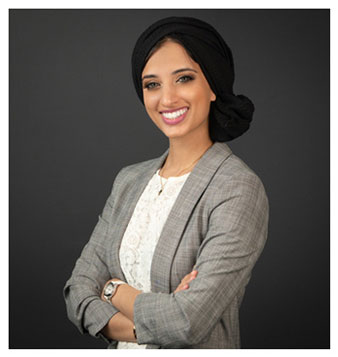
Dr. Sarah Ahmed, M.D.
Sarah Farukhi Ahmed, MD is an ophthalmologist and glaucoma surgeon. She graduated Magna Cum Laude from the University of ..

Dr. Noor Amra, M.D.
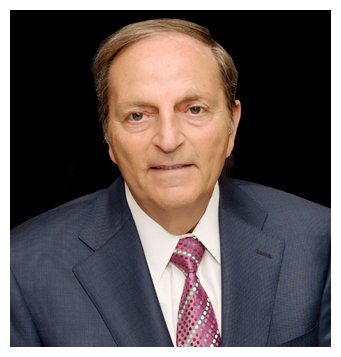
R.K. Ghosheh, M.D.


I wanted to thank you so much for helping my eyes to see and feel better. I was afraid of any kind of eye surgery but other friends said you were the best doctor around. You’re nurses were the nicest nurses I have ever had and your front desk staff was so nice. Thank you again and God bless all of you…
Letters Written to Dr. Ghosheh and Advance Medical Group

About six or seven years ago I was referred to you by a friend of mine who had Lasik done at your facility. She was very impressed so I came to see you. When I had my consult with another doctor I decided to have my eyes done because with the vision I had, I was miserable. Thank you for being a great guy.
Dear Dr. R.K. Ghosheh,

Words cannot express the amazing gift of sight that you have provided me. I have been struggling to see for years with glasses and/or contacts. I never thought it would be possible to see so nicely without them. What a wonderful profession to be apart of… giving the gift of sight. Thank all of you.
Dear Dr. Ghosheh
Designation: CEO






